Dr. Pedro Alarcón Goldenberg, an Endodontics specialist and professor at the University of Valparaíso, Chile, presents a clinical case of a 57-year-old patient with a history of previous surgery (curettage) performed 4 years ago on teeth 1.4 and 1.5, resulting in a scar on the vestibular area.
Diagnosis
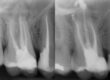
The patient presented with radiating pain to the cheek area and symptoms persisting for the past 4 months. The diagnosis revealed symptomatic apical periodontitis related to the upper premolars on the right side. These teeth had undergone previous endodontic treatment and were crowned with cast post and core anchors in the canals.
A periapical X-ray was taken, and a CBCT scan was requested to plan the paraendodontic surgery with retrograde filling due to the high risk of crown and post removal leading to fracture. The patient experienced symptoms for several months, including pain upon palpation and positive vertical percussion test.
Upon flap elevation, granulation tissue and fibrosis adhered to the mucosa were observed and carefully detached using a no. 15C blade. The procedure started with the removal of inflammatory tissue using curettes, exposing the extensive lesion on tooth 1.5. Osteotomy was then performed on both premolars to achieve direct access to the root apices.
- Previous
- Fibrous injury
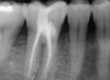
Next, a 3mm apical resection (apicectomy) was performed, providing a direct view of the apices. After separating the apical end, the canals were located using methylene blue staining, followed by retrograde preparation. Tooth 1.4 had two roots, vestibular and palatal, while tooth 1.5 had a well-filled and oval-shaped canal.
- US preparation
- Staining and cones
Once the retrograde cavities were shaped using ultrasonic tips, retrograde filling was carried out using Zarc’s NeoPutty, a reparative bioceramic cement known for its remarkable bioactive properties. It is resin-free, does not discolor teeth, and comes pre-mixed with a consistency that allows for easy manipulation. Its high radiopacity (8.4mm Al) enables good radiographic discrimination and follow-up. The material was placed and compacted in the retro-cavities of the root canals.
Due to aesthetic considerations and the presence of metal-ceramic crowns with prosthetic restoration, including a post obstructing access to the apical third, apical surgery was chosen as the therapeutic approach.
- NeoPutty application
- Retro-preparation
- Allograft
- L-PRF membrane
To promote guided bone regeneration in the treated area, the cavity was filled with allograft bone tissue and autogenous L-PRF membranes were placed over the surgical site. Finally, the flap was repositioned and sutured with 5.0 Nylon.

Sutures
There has been debate about the need for filling the surgical site after root end resection. Some studies have shown that healing occurs regardless of whether bone grafting is performed, but it does promote and accelerate bone regeneration

Follow-up X-ray
In the past, paraendodontic surgery was considered a desperate and last-resort procedure with unpredictable results due to limited understanding of endodontic pathology and treatment failure causes.
The development of new instruments, microsurgical techniques, improved lighting, magnification, and the introduction of new materials for sealing the root end have revolutionized endodontic surgery, significantly improving outcomes and prognosis. With careful case selection and the skills of the surgeon, periradicular surgery can be considered a predictable alternative, weighing the cost-benefit of tooth extraction and subsequent replacement.
More information
If you are interested in trying our products, please contact us via email at hola@zarc4endo.com. We will be delighted to assist you!